How to Track Ovulation with PCOS

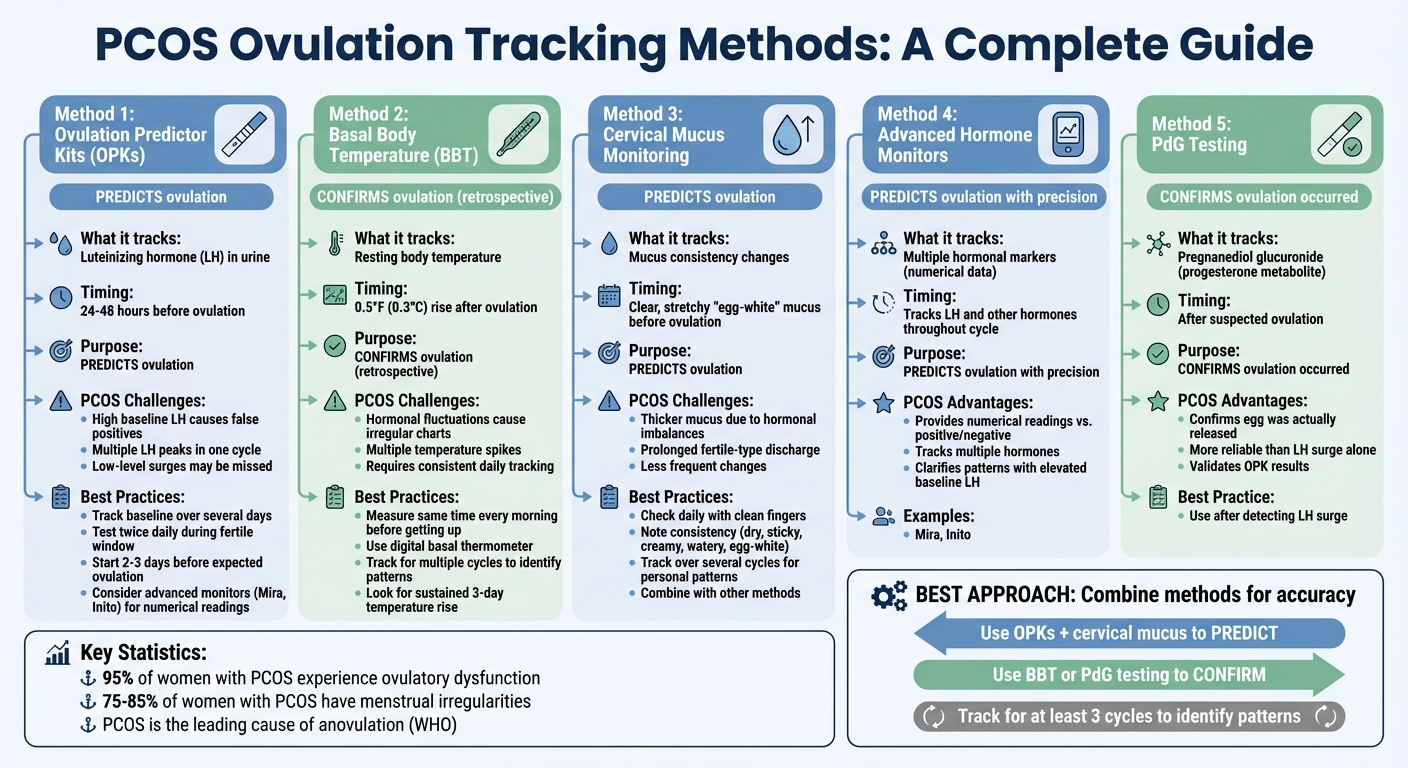
PCOS makes tracking ovulation tricky due to hormonal imbalances and irregular cycles. Tools like ovulation predictor kits (OPKs), basal body temperature (BBT) tracking, and cervical mucus monitoring can help, but they often require adjustments for accuracy. For example, high baseline LH levels may cause false positives with OPKs, and hormonal fluctuations can make BBT patterns hard to interpret. Combining multiple methods - like using OPKs to predict ovulation and BBT or PdG testing to confirm it - offers a clearer picture of your fertility. Consistency is key: track over several cycles to identify patterns, and consider advanced hormone monitors if traditional tools feel unreliable. If irregularity persists, consult a healthcare provider for tailored guidance.
How PCOS Affects Ovulation
How PCOS Disrupts Ovulation
PCOS interferes with ovulation through hormonal imbalances that prevent the proper release of eggs. Elevated levels of androgens (male hormones like testosterone) can stop the ovaries from releasing mature eggs. On top of that, insulin resistance - a common issue in PCOS - further boosts androgen production, creating a hormonal cycle that disrupts follicle development.
"High androgen levels prevent your ovaries from releasing eggs, which causes irregular menstrual cycles." - Cleveland Clinic [10]
Instead of producing one dominant follicle ready for ovulation, the ovaries in individuals with PCOS often generate multiple immature follicles. This condition leads to ovulatory dysfunction in up to 95% of women with PCOS [9]. The World Health Organization even recognizes PCOS as the leading cause of anovulation and infertility [12].
As a result, between 75–85% of women with PCOS experience noticeable menstrual irregularities [11]. These irregularities might show up as infrequent or unpredictable periods. The hormonal disruptions not only make egg maturation difficult but also complicate efforts to track ovulation using conventional methods.
Why Tracking Ovulation Is Harder with PCOS
Tracking ovulation is particularly tricky for those with PCOS due to the hormonal disruptions it causes. For instance, many individuals with PCOS have elevated baseline levels of luteinizing hormone (LH). Since ovulation predictor kits (OPKs) are designed to detect an LH surge around 25 mIU/mL, a high baseline LH level can lead to false positives, making it seem like ovulation is happening when it’s not.
"High LH is one common sign of PCOS, so it's not uncommon for PCOS patients to have a positive LH result on urine tests - but that doesn't necessarily mean that it's an LH surge associated with ovulation." - Bird&Be Editorial Team [7]
Physical signs of ovulation can also be unreliable. Normally, basal body temperature (BBT) rises by 0.9–1.8°F after ovulation due to increased progesterone. However, with PCOS, hormonal fluctuations can make BBT patterns unpredictable. Similarly, cervical mucus, which typically becomes thinner and stretchier before ovulation, may remain thick and sticky because of lower estradiol levels. Even cycle-tracking apps, which often assume a regular 28-day cycle, can be inaccurate for those with PCOS since ovulation may occur much later - or not at all - in the cycle.
Fertility Charting - PCOS | Ovulation Tracking | Pregnancy Chart PCOS
Methods for Tracking Ovulation with PCOS
PCOS Ovulation Tracking Methods Comparison Chart
Using Ovulation Predictor Kits (OPKs)
Ovulation predictor kits (OPKs) work by detecting luteinizing hormone (LH) in your urine, which typically spikes 24 to 48 hours before ovulation [13]. For those with PCOS, though, using OPKs requires a slightly different approach due to hormonal irregularities. To get accurate results, track your LH levels over several days to identify your personal baseline and distinguish between minor fluctuations and a true surge [13]. Testing in the afternoon is recommended, as LH levels are often more detectable later in the day [1]. Start testing two to three days before your estimated ovulation date (based on your shortest cycle) and test twice daily during your fertile window to catch any brief surges [1].
"PCOS may result in false positives, so it's important to track OPK results alongside other methods for accuracy." - Zora Health [1]
Keep in mind that OPKs predict ovulation attempts but don’t confirm that an egg was released [13]. If standard kits feel unreliable, advanced monitors like Mira or Inito can provide numerical hormone readings, offering a clearer picture of your unique patterns [13].
| Challenge with PCOS | Impact on OPK Results | Recommended Strategy |
|---|---|---|
| High Baseline LH | Frequent false positives | Track your baseline; consider advanced monitors for precise readings. |
| Multiple LH Peaks | Multiple "surges" in one cycle | Continue testing after the first surge; confirm ovulation using BBT or PdG testing. |
| Irregular Cycles | Uncertainty about when to start testing | Start early (2-3 days before your earliest expected fertile window) and test twice daily. |
| Low-Level Surges | Missed surges due to low thresholds | Use low-threshold tests or digital monitors for better accuracy. |
Charting Basal Body Temperature (BBT)
When OPK results are unclear, charting your basal body temperature (BBT) can confirm ovulation retrospectively. BBT is your body’s lowest resting temperature, measured first thing in the morning [1]. After ovulation, progesterone causes a slight temperature rise - about 0.5°F (0.3°C) [1]. Unlike OPKs, BBT confirms ovulation has occurred rather than predicting it [3]. For women with PCOS, BBT is most effective when used alongside other tracking methods [1].
Use a digital basal thermometer and take your temperature at the same time every morning before getting out of bed [1]. Record your readings in a fertility app or on paper to track the subtle temperature shift over time [1]. PCOS-related hormonal fluctuations can result in irregular charts with multiple spikes, so consistency and long-term tracking are key to identifying patterns [1].
"If you don't do it every day, you can easily miss the slight rise in temperature. So to be successful with this method you must be consistent." - Kelly, PCOS Advocate, PCOS Living [8]
Factors like stress, alcohol, illness, or disrupted sleep can affect your BBT readings [3]. If daily manual tracking feels overwhelming, devices like OvuSense offer continuous core temperature monitoring with claims of high accuracy for pinpointing ovulation dates [8].
Monitoring Cervical Mucus
Cervical mucus changes throughout your cycle, offering another way to track ovulation. As ovulation nears, mucus often becomes clear, slippery, and stretchy, resembling raw egg whites [4]. During non-fertile phases, it’s typically dry, sticky, or thick [8]. With PCOS, hormonal imbalances can cause thicker mucus or prolonged "fertile-type" discharge [4] [14].
Check your mucus daily using clean fingers or toilet paper, and note its consistency (e.g., dry, sticky, creamy, watery, or egg-white) [4] [8]. The most fertile period is marked by mucus that is stretchy and slippery [4]. After ovulation, mucus usually becomes dry again [14].
"Women with PCOS may experience thicker cervical mucus or less frequent changes due to hormonal imbalances. Tracking this, along with other methods, can help improve the accuracy of your ovulation prediction." - Anna Haotanto, Founder, Zora Health [4]
Tracking cervical mucus over several cycles can help you identify your personal patterns. Combining this method with BBT or hormone monitoring can further confirm ovulation [4].
Advanced Hormone Monitors
For those who find traditional methods inconclusive, advanced hormone monitors like Mira and Inito offer a more detailed approach. These devices track multiple hormonal markers and provide numerical data instead of simple positive/negative results [13]. By measuring not just LH but also other ovulation-related hormones, they can help clarify patterns, especially for women with elevated baseline LH or irregular surges. Tracking over several cycles with these tools can offer deeper insights into your fertility.
PdG Testing for Ovulation Confirmation
To confirm ovulation after detecting an LH surge, PdG (pregnanediol glucuronide) testing can be a reliable option. PdG, a urine metabolite of progesterone, indicates that ovulation has occurred [13]. This step is particularly helpful for women with PCOS, as an LH surge doesn’t always result in ovulation. By combining OPKs to predict ovulation with PdG testing to confirm it, you can gain more confidence in identifying whether an egg was released.
Combining Multiple Tracking Methods
When managing PCOS, relying on just one tracking method often doesn’t cut it. Using multiple tools together gives you a much clearer view of your cycle. Ovulation predictor kits (OPKs) and cervical mucus changes can help predict when ovulation might occur, but basal body temperature (BBT) confirms that ovulation actually happened by detecting the temperature rise caused by progesterone [1][8]. This combination is crucial because up to 95% of women with PCOS experience ovulatory dysfunction [9]. In these cases, your body might show signs of attempting ovulation without actually releasing an egg. Layering these methods step-by-step during your fertile window can make all the difference.
To get started, check your cervical mucus daily and use OPKs during your suspected fertile window - this is usually a few days after your period ends. When you notice “egg-white” cervical mucus or detect an LH surge with an OPK, continue tracking your BBT every morning at the same time. The idea is to use OPKs and mucus changes to predict ovulation, then confirm it with a sustained BBT rise. A temperature increase of about 0.5°F to 1.0°F (0.3°C to 0.6°C) that stays elevated for at least three days is a strong indicator that ovulation occurred [1][5][6]. This pattern reflects a progesterone increase, confirming that an egg was released, not just that your body tried to ovulate.
If OPKs frequently give false positives - a common issue with PCOS - pairing them with BBT or PdG testing can help. Unlike OPKs, which detect LH surges, PdG tests measure progesterone levels, offering more precise confirmation of ovulation. This two-step approach - predicting ovulation with LH and confirming it with PdG or BBT - can help you navigate the false positives that PCOS often throws into the mix.
For the best results, track your data across at least three cycles to spot patterns. As Dr. Erin Higgins from Cleveland Clinic explains: "Sometimes, patients feel like their cycles are totally unpredictable, but when we take a step back, they really only vary by a couple of days" [6]. Logging all this information in a fertility app makes it easier to identify trends and provides your healthcare provider with valuable insights if you need further assistance.
Conclusion
Fine-tuning your tracking strategy can make a big difference when managing ovulation with PCOS. Since PCOS often leads to elevated baseline LH levels, relying on just one tracking method can result in confusion or false positives [1][2]. A multi-method approach is key.
Consistency is crucial. Track for at least three cycles to identify your unique patterns. Make it a habit to record your basal body temperature (BBT) and monitor cervical mucus daily. If needed, test LH levels twice a day during your fertile window [3].
"Tracking ovulation is especially important for women with PCOS. It may take time and a combination of methods to find what works best for you, but consistency is key to understanding your body's fertility patterns." – Anna Haotanto, Founder, Zora Health [1]
Patience is also essential. Your body might show signs of attempted ovulation without actually releasing an egg. That's where confirmation methods like BBT or PdG testing become invaluable. Over time, these efforts will help reveal your body's patterns more clearly.
If irregular cycles persist - even after consistent tracking - or if you're experiencing fewer than 10 periods a year, it's time to consult your healthcare provider [3]. They can perform ultrasounds to monitor follicle development or discuss medications like Clomid to help stimulate ovulation [1][2]. Your tracking efforts can provide your doctor with detailed insights, helping them create a treatment plan tailored to your needs.
For more tips and personalized guidance on managing PCOS, visit mypcoslife.com.
FAQs
What are the best ways to track ovulation with PCOS?
Tracking ovulation when dealing with PCOS can feel tricky because of irregular cycles, but using multiple methods together can make it easier to pinpoint fertile days.
Ovulation predictor kits (OPKs) work by detecting the LH surge that typically happens before ovulation. However, with PCOS, these kits might not always be reliable. To improve your chances, start testing earlier in your cycle and consider testing twice a day. This approach gives you a better shot at catching the surge.
Another helpful method is basal body temperature (BBT) tracking. By monitoring your temperature daily, you can spot a slight increase that occurs after ovulation. While this confirms ovulation has happened, it doesn’t predict it, so it’s best used alongside other methods.
Paying attention to cervical mucus changes can also provide clues. Fertile mucus tends to be clear and stretchy, resembling raw egg whites. That said, PCOS can sometimes make these signs less predictable, so it’s important to combine this with other tracking tools.
Keeping a detailed log of your symptoms, cycle patterns, and tracking results over time can reveal patterns unique to your body. For extra support and tailored advice, it’s always a good idea to work with your healthcare provider. They can help you make the most of these methods and adapt them to your situation.
How can I tell if my ovulation tracking methods aren’t working with PCOS?
If you're finding that your ovulation tracking methods aren't giving you reliable results, there are a few signs to watch for. These might include irregular or completely absent ovulation patterns, no clear shifts in your basal body temperature, consistently negative readings from ovulation predictor kits, or cycles that remain irregular despite your tracking efforts.
For those with PCOS, hormonal imbalances can often interfere with traditional tracking methods, making them less dependable. If these challenges sound familiar, it might be time to consult a healthcare provider. They can offer personalized advice and suggest alternative tracking strategies designed specifically for managing PCOS.
When should I see a doctor about difficulties tracking ovulation with PCOS?
If tracking ovulation feels like a challenge due to PCOS, reaching out to a healthcare provider is a smart move - particularly if your cycles are consistently irregular or you suspect ovulation isn’t happening. They can help pinpoint any underlying issues and suggest treatments that support your reproductive health.
For those trying to conceive without success after several months of tracking, a doctor can create a personalized plan to tackle potential fertility hurdles. Getting professional guidance ensures you're on the right path toward achieving your health and family planning goals.
